Orthokeratology (Ortho-K) in Malaysia
Orthokeratology, commonly known as Ortho-K or corneal refractive therapy, has become an innovative, non-surgical solution to temporarily correct myopia and slow its progression, especially in children. Ortho K therapy involves wearing rigid gas permeable (RGP) contact lenses—known as ortho K lenses—overnight. These lenses gently reshape the cornea, correcting refractive errors to allow for clear, natural vision throughout the day without needing to wear glasses or contact lenses. Orthokeratology, or Ortho-K, has emerged as an innovative non-surgical intervention designed to temporarily correct myopia and slow its progression, particularly in children. Ortho-K involves the use of specially designed gas-permeable contact lenses that are worn overnight. These lenses gently reshape the cornea, temporarily altering its curvature to correct refractive errors and provide clear vision during the day without the need for glasses or contact lenses [2] [4] [10].

Studies reveal that Ortho-K is the most successful method in myopia control. A meta-analysis of randomized controlled trials indicated that Ortho-K can effectively slow axial elongation in myopic children, which is a key factor in myopia progression [8]. The treatment has been shown to reduce axial elongation by approximately 43% compared to children wearing single-vision glasses [1]. It is effective for children with moderate astigmatism, showcasing its versatility in myopia management [10].
Despite its benefits, Ortho-K is not without risk as with any contact lens wear. Nevertheless, these risks are minimal and can be efficiently mitigated by adhering to scheduled follow-up appointments, maintaining strict compliance with cleaning routines, and using suitable solutions to safeguard the wearer’s well-being. The safety and efficacy of Ortho-K necessitate careful patient selection, education, and regular follow-up with experienced eye care professionals to minimise potential complications and ensure optimal outcomes [4] [5] [7].
What is Myopia and Its Prevalence?
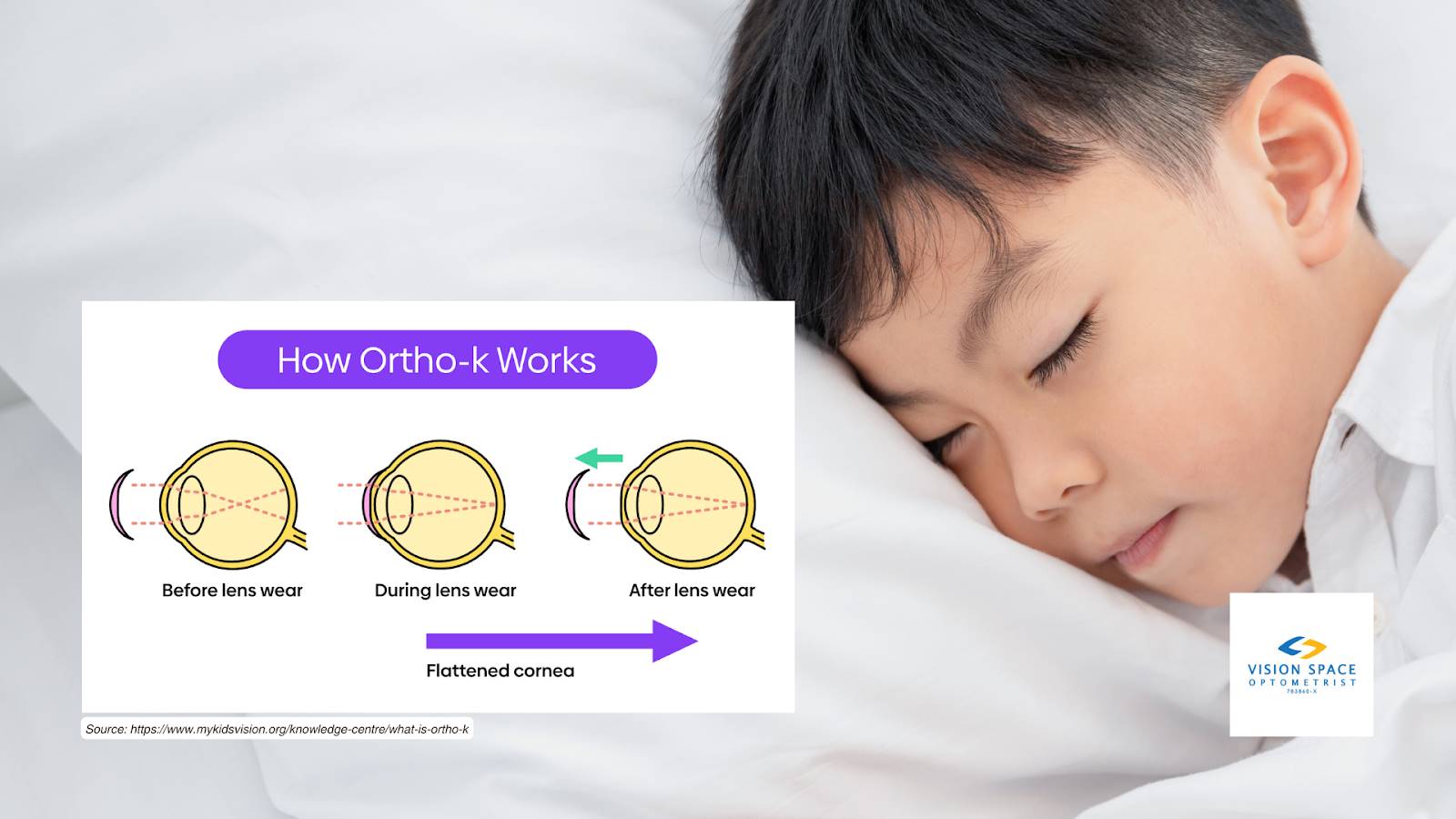
Myopia, often referred to as shortsightedness, is a vision condition characterised by the blurring of distant objects while nearby objects remain sharp and clear. This issue arises when the length of the eyeball is disproportionately long compared to the cornea and lens’s ability to focus, leading to the convergence of light rays before they reach the retina. Myopia is a significant and growing public health concern, with its prevalence increasing rapidly across the globe. Estimates suggest that by 2050, nearly half of the world’s population may be affected by myopia.
The rising prevalence of myopia is attributed to a combination of genetic and environmental factors, including increased near work activities, such as reading and screen time, and reduced time spent outdoors [3] [6]. Urbanisation and lifestyle changes have also been implicated in the myopia epidemic, particularly in East Asian countries where the condition affects a substantial proportion of children and adolescents [3] [9].
Understanding Ortho-K
Orthokeratology, commonly referred to as Ortho-K, is a non-surgical procedure that temporarily corrects refractive errors by reshaping the cornea. This section delves into the mechanism of Ortho-K and the scientific principles that enable overnight corneal reshaping to improve vision temporarily.
Explanation of How Ortho-K Works to Reshape the Cornea
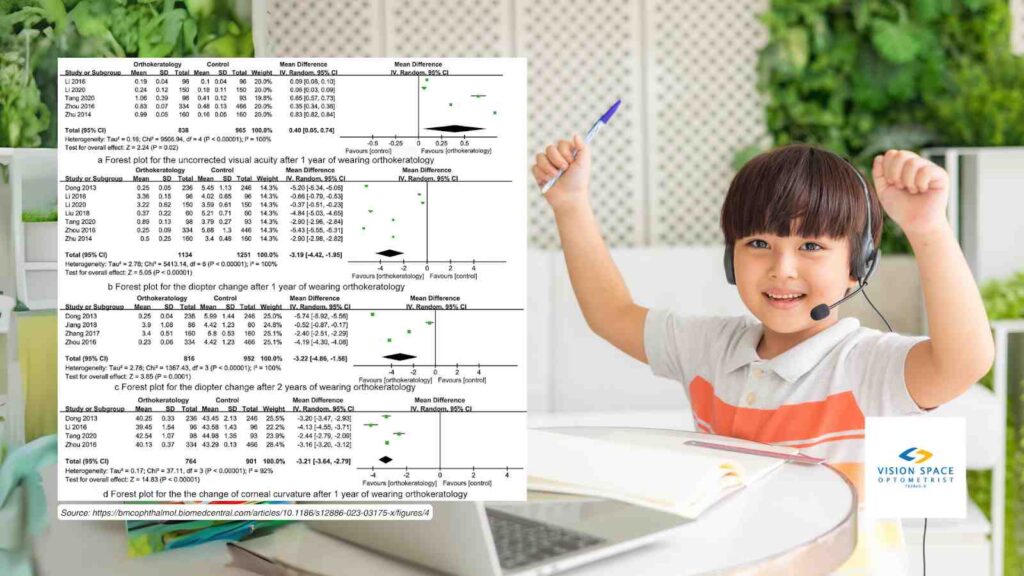
Ortho-K utilises specially designed gas permeable contact lenses that are worn overnight. These lenses apply gentle pressure to the cornea, which is the clear, dome-shaped front surface of the eye responsible for focusing light onto the retina. The cornea’s shape is crucial in determining how well the eye can focus light and, consequently, how clear the vision is.
The process begins with a comprehensive eye examination where an eye care professional takes precise measurements of the cornea using an instrument called a corneal topographer. This device creates a detailed map of the eye’s surface, which is then used to design custom contact lenses tailored to the individual’s corneal shape [11] [12] [13].

When the Ortho-K lenses are worn during sleep, they act to flatten the central cornea by redistributing the epithelial cells, which are the outermost cells of the cornea. This redistribution is facilitated by the tear film that is trapped between the lens and the cornea. The pressure exerted by the lens causes the central cornea to flatten while maintaining the health of the corneal tissue due to the high oxygen permeability of the lenses [11] [12] [13].
The Science Behind Overnight Corneal Reshaping and Its Temporary Effects on Vision
The temporary vision correction achieved with Ortho-K is a result of the cornea’s elastic properties. The cornea is composed of collagen fibres and cells that can be molded under pressure but will gradually return to their original shape once the pressure is removed. This is why the effects of Ortho-K are reversible and require the lenses to be worn regularly to maintain the corrected vision [11] [12] [13].
During the night, the Ortho-K lenses reshape the cornea’s curvature, correcting refractive errors such as myopia (nearsightedness) and astigmatism. By the morning, when the lenses are removed, the cornea retains the new shape for a period, typically providing clear vision throughout the day without the need for glasses or daytime contact lenses [11] [12] [13].
The temporary nature of the vision correction is due to the cornea’s tendency to revert to its original shape over time. This is why consistent nightly wear of the Ortho-K lenses is necessary to sustain the desired vision correction. The cornea’s ability to revert back to its original shape also means that Ortho-K is a reversible procedure, and if lens wear is discontinued, the cornea will return to its pre-treatment curvature, and the refractive error will reappear [11] [12] [13].
Effectiveness of Ortho-K in Myopia Control
Summary of Recent Studies Highlighting Ortho-K’s Impact on Controlling Myopia Progression
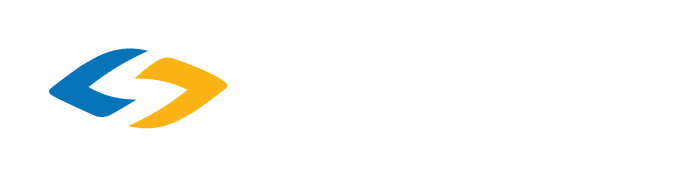
Recent studies have continued to evaluate the effectiveness of orthokeratology (Ortho-K) in controlling the progression of myopia in children and adolescents. A meta-analysis of randomised controlled trials published in 2023 assessed the role of Ortho-K in controlling myopia in children and concluded that Ortho-K improved uncorrected visual acuity, reduced diopter change, changes of corneal curvature, the length of ocular axis, and the amount of ocular axis change after 1 and 2 years of wearing Ortho-K lenses [20]. This suggests that Ortho-K can effectively delay the progression of myopia in children, although the long-term effects require further investigation.
Another study, the “Effectiveness of Orthokeratology in Myopia Control,” reported that Ortho-K, when used for partial or full correction of myopia, has been shown to slow myopic progression in children by 36-56% compared to their spectacle or contact-lens wearing peers [17]. This study also highlighted the importance of early intervention, especially in high myopes and children, where myopic progression tends to be faster.
The “Ortho-K Effectiveness Wanes Over Time, Study Concludes” article from 2023 discussed a systematic review and meta-analysis that evaluated Ortho-K at different time points over a two-year period. The analysis determined that Ortho-K could effectively reduce axial length (AL) elongation in myopic children within six months, with a prolonged effect up to 24 months [14].
The “Retardation of Myopia in Orthokeratology (ROMIO) Study” was a 2-year randomized clinical trial that aimed to evaluate the effectiveness of Ortho-K for myopic control. The research indicated that individuals using Ortho-K lenses experienced a 43% reduction in the rate of axial elongation compared to those using standard single-vision spectacles. [15].
Discussion on the Significance of Controlling Myopia in Children and Adolescents
Controlling myopia in children and adolescents is of significant importance due to the potential long-term health implications associated with high myopia. Myopia, particularly when it progresses to high levels, is associated with an increased risk of sight-threatening conditions such as retinal detachment, choroidal degeneration, cataracts, and glaucoma [18] [19]. By slowing the progression of myopia, interventions like Ortho-K can potentially reduce the risk of these complications and improve the overall quality of life for affected individuals.
Furthermore, myopia typically starts developing before age 10 and then progresses or worsens every few months in children and teenagers [16]. Interventions that can slow down this progression can have a substantial impact on the visual outcomes of these individuals. Ortho-K lenses, which are worn overnight to temporarily reshape the cornea, have been shown to be an effective non-surgical option for controlling myopia progression in the pediatric population.
The significance of controlling myopia also extends to the social and educational aspects of a child’s life. Better vision can lead to improved academic performance and participation in activities, which are crucial during the formative years. Additionally, by potentially reducing the dependence on corrective eyewear, children may experience enhanced self-esteem and social interactions.
References:
[1] Cho, Pauline, and Sin-Wan Cheung. “Retardation of Myopia in Orthokeratology (ROMIO) Study: A 2-Year Randomized Clinical Trial.” Investigative Ophthalmology & Visual Science, vol. 53, no. 11, 2012, pp. 7077-7085. https://iovs.arvojournals.org/article.aspx?articleid=2127470. Accessed 30 Mar. 2024.
[2] “Ortho-K for Myopia Control.” MyKidsVision.org, https://www.mykidsvision.org/knowledge-centre/ortho-k-for-myopia-control. Accessed 30 Mar. 2024.
[3] Mehta, Neesurg, and Angie Wen. “Myopia: A Global Epidemic. An Overview of the Problem and Efforts to Address It.” Retina Today, Sep. 2019, https://retinatoday.com/articles/2019-sept/myopia-a-global-epidemic. Accessed 30 Mar. 2024.
[4] Low, Yu Chen, et al. “Peripheral Eye Length Evaluation in Myopic Children Undergoing Orthokeratology Treatment for 12 Months Using MRI.” Clinical Optometry, vol. 16, 9 Feb. 2024, pp. 35-44, doi:10.2147/OPTO.S448815. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10863466/. Accessed 30 Mar. 2024.
[5] Gifford, Kate. “The Latest Research on Orthokeratology: Compliance, Safety, Comfort and Combination with Atropine.” MyopiaProfile.com, 30 Aug. 2021, https://www.myopiaprofile.com/articles/the-latest-research-on-orthokeratology. Accessed 30 Mar. 2024.
[6] Zhang, XJ, et al. “Prevalence of Myopia in Children Before, During, and After COVID-19 Restrictions in Hong Kong.” JAMA Network Open, vol. 6, no. 3, 2023, e234080. JAMA Network, https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2802737. Accessed 30 Mar. 2024.
[7] Lee, Yueh-Chang, et al. “Effect of Orthokeratology on Myopia Progression: Twelve-Year Results of a Retrospective Cohort Study.” BMC Ophthalmology, vol. 17, no. 1, 2017, art. 243, doi:10.1186/s12886-017-0639-4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5721542/. Accessed 30 Mar. 2024.
[8] Li, X., Xu, M., San, S., et al. “Orthokeratology in Controlling Myopia of Children: A Meta-Analysis of Randomized Controlled Trials.” BMC Ophthalmology, vol. 23, 441 (2023), https://doi.org/10.1186/s12886-023-03175-x. Accessed 30 Mar. 2024.
[9] “New Center Tackles Rapidly Growing Myopia Prevalence.” Stanford University Department of Ophthalmology Annual Report 2021, Stanford University, 2021, https://med.stanford.edu/ophthalmology/news-and-media/annualreport_2021/myopia.html. Accessed 30 Mar. 2024.
[10] Chen, Connie, Sin Wan Cheung, and Pauline Cho. “Myopia Control Using Toric Orthokeratology (TO-SEE Study).” Investigative Ophthalmology & Visual Science, vol. 54, Oct. 2013, pp. 6510-6517, https://doi.org/10.1167/iovs.13-12527. Accessed 30 Mar. 2024.
[11] Heiting, Gary. “Orthokeratology: Ortho-K and CRT Contact Lenses for Myopia.” All About Vision, 27 Feb. 2019, https://www.allaboutvision.com/contacts/orthok.htm. Accessed 30 Mar. 2024.
[12] “What Is Ortho-K?” MyKidsVision.org, https://www.mykidsvision.org/knowledge-centre/what-is-ortho-k. Accessed 30 Mar. 2024.
[13] “What Is Orthokeratology?” American Academy of Orthokeratology and Myopia Control, https://aaomc.org/what-is-orthokeratology/. Accessed 30 Mar. 2024.
[14] “Ortho-K Effectiveness Wanes Over Time, Study Concludes.” Review of Optometry, https://www.reviewofoptometry.com/article/orthok-effectiveness-wanes-over-time-study-concludes. Accessed 30 Mar. 2024.
[15] Cho, Pauline, and Sin-Wan Cheung. “Retardation of Myopia in Orthokeratology (ROMIO) Study: A 2-Year Randomized Clinical Trial.” Investigative Ophthalmology & Visual Science, vol. 53, no. 11, Oct. 2012, pp. 7077-7085, https://doi.org/10.1167/iovs.12-10565. Accessed 30 Mar. 2024.
[16] “What Is Myopia Control and Why It’s Important.” MyKidsVision.org, https://www.mykidsvision.org/knowledge-centre/what-is-myopia-control-and-why-its-important. Accessed 30 Mar. 2024.
[17] Harthan, Jennifer OD, Illinois College of Optometry. “Effectiveness of Orthokeratology in Myopia Control.” ClinicalTrials.gov, Illinois College of Optometry, Wesley Research Institute, 14 Mar. 2018, last update 28 Sep. 2023, NCT03465748, https://classic.clinicaltrials.gov/ct2/show/NCT03465748. Accessed 30 Mar. 2024.
[18] Smith, Molly J., and Jeffrey J. Walline. “Controlling Myopia Progression in Children and Adolescents.” Adolescent Health, Medicine and Therapeutics, vol. 6, 2015, pp. 133-140, doi:10.2147/AHMT.S55834. https://pubmed.ncbi.nlm.nih.gov/26316834/. Accessed 30 Mar. 2024.
[19] Porter, Daniel. “Myopia Control in Children.” American Academy of Ophthalmology, 15 Nov. 2022, www.aao.org/eye-health/diseases/myopia-control-in-children. Accessed 30 Mar. 2024.
[20] Li, Xue, et al. “Orthokeratology in Controlling Myopia of Children: A Meta-Analysis of Randomized Controlled Trials.” BMC Ophthalmology, vol. 23, no. 441, 31 Oct. 2023, bmcophthalmol.biomedcentral.com/articles/10.1186/s12886-023-03175-x. Accessed 30 Mar. 2024.