Introduction: Understanding Tonometry and Glaucoma in the Elderly in Malaysia
The Silent Threat of Glaucoma
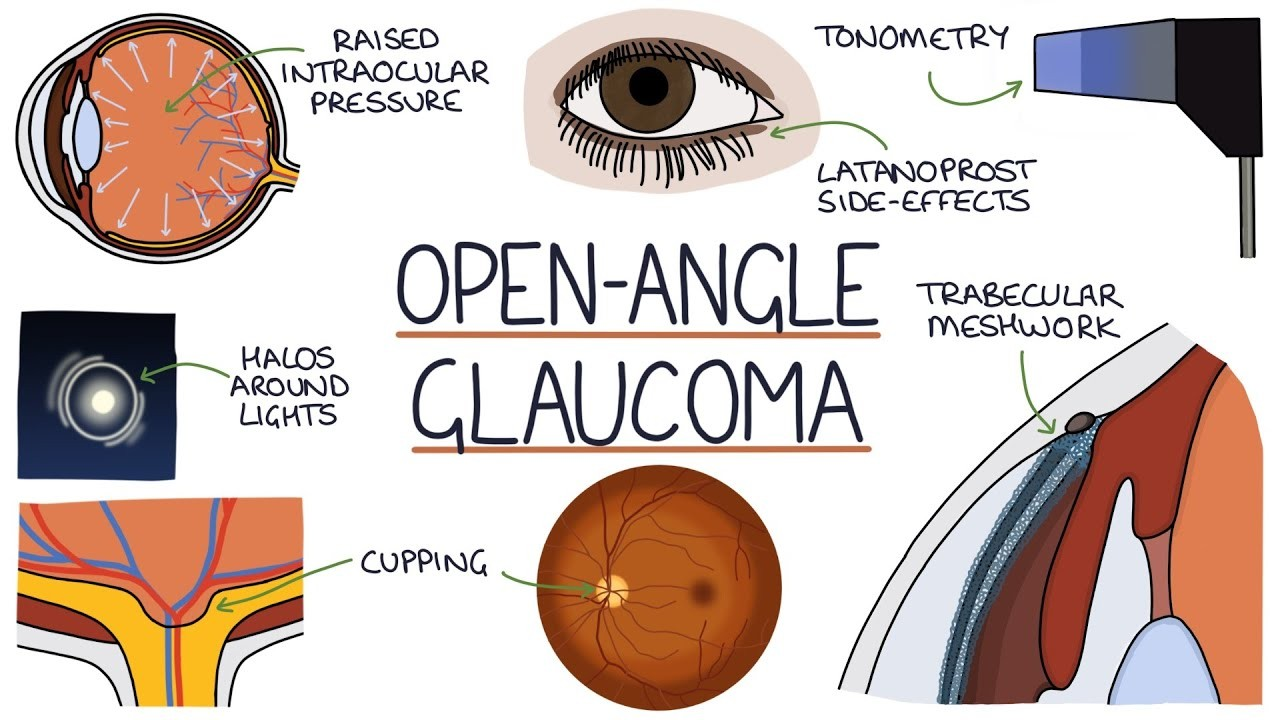
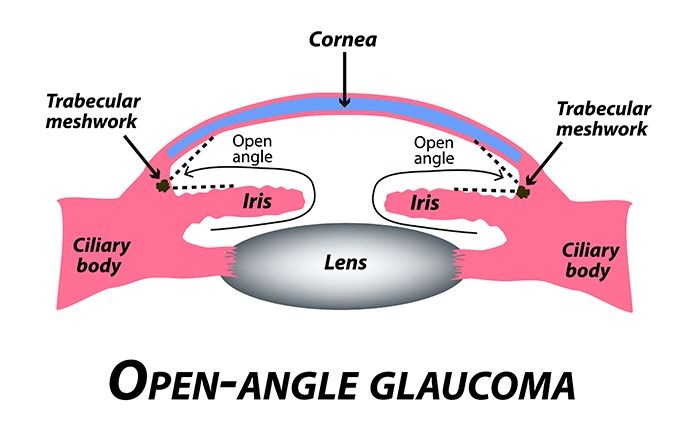
Glaucoma is a leading cause of irreversible blindness worldwide, often progressing without noticeable symptoms until significant vision loss occurs. It primarily affects the optic nerve when intraocular pressure (IOP) within the eye escalates, harming the delicate nerve fibers that are crucial for vision.
In Malaysia, a study indicated that the prevalence of visual impairment and blindness in the elderly is significant, with glaucoma being a major contributing factor. This underscores the critical nature of early detection and regular monitoring (Chew et al., 2018) [1].
Understanding Tonometry: A Key Diagnostic Tool
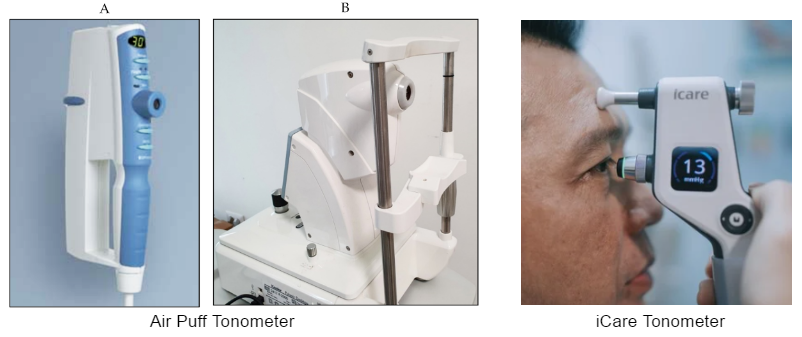
Tonometry is an essential diagnostic tool that specifically measures the pressure inside your eye, crucial for detecting glaucoma early by assessing the risk associated with elevated eye pressure. Among the different types of tonometry, air puff tonometry is notable for its non-invasive nature, where a quick burst of air is used to gauge the eye’s resistance to pressure. This method is particularly beneficial for the elderly, providing a discomfort-free experience without the need for direct eye contact, making it ideal for regular screenings.
Another variety of non-contact tonometer is the iCare. This rebound tonometer introduces a fresh approach to measuring intraocular pressure (IOP). It involves gently propelling a lightweight probe onto the corneal surface, which then quickly recoils. The iCare has garnered considerable attention in clinical practice due to its comfort and user-friendly nature [2].
Tonometry and Its Role in Glaucoma Diagnosis
Tonometry is a diagnostic procedure that measures the pressure inside the eye, specifically the intraocular pressure (IOP). This measurement is crucial for diagnosing and managing glaucoma, as elevated IOP is a significant risk factor for this condition, which can lead to optic nerve damage and, ultimately, vision loss. The most common types of tonometry include Goldmann applanation tonometry, non-contact tonometry (air puff tonometer and icare tonometer), Schiotz tonometry, pneumotonometer, and Tono-Pen. Among these, Goldmann applanation tonometry is widely regarded as the gold standard due to its accuracy in measuring the force necessary to flatten a corneal area of 3.06mm diameter.
Glaucoma in Malaysia: A Look at the Statistics
Recent studies in Malaysia reveal concerning statistics about glaucoma’s prevalence and the general eye health of the elderly. According to the National Eye Survey in Malaysia (NESII), the prevalence of glaucoma among the elderly is notably high, with significant impacts on their quality of life. The study emphasizes the necessity for targeted screening and enhanced ophthalmological services to manage this condition effectively and prevent blindness (Chew et al., 2018) [1].
The Importance of Regular Screening in the Elderly
Regular screening for glaucoma is vital, particularly for the elderly population, as early detection can drastically alter the course of the disease. A study highlighted that the prevalence of glaucoma increases with age, making the elderly a key demographic for regular eye health assessments. Effective screening can lead to early intervention, significantly reducing the risk of severe visual impairment and maintaining a higher quality of life (Chew et al., 2018) [1].
References
- [1] Chew, F., et al. “Estimates of visual impairment and its causes from the National Eye Survey in Malaysia (NESII).” PLOS ONE, vol. 13, no. 6, 2018, e0198799. [https://dx.doi.org/10.1371/journal.pone.0198799].
- [2] Chen, M., et al. “Comparability of Three Intraocular Pressure Measurements: iCare Pro Rebound, Non-Contact, and Goldmann Applanation Tonometry in Different IOP Groups.” BMC Ophthalmology, vol. 19, 2019, article 225, https://doi.org/10.1186/s12886-019-1236-5.
II. The Necessity of Intraocular Pressure Screening in the Elderly in Malaysia
Understanding Tonometry’s Role in Eye Health
Tonometry is pivotal in assessing intraocular pressure (IOP), a key indicator of glaucoma risk. It specifically assesses the pressure of your eye, underlining its importance in early glaucoma detection. Among the methods available, air puff tonometry provides a non-contact, pain-free testing experience that is well-suited for elderly patients. By measuring the cornea’s response to a burst of air, this method quickly and effectively gauges eye pressure, offering a critical early warning for those at risk of developing glaucoma.
High Prevalence of Glaucoma Among the Elderly
In Malaysia, glaucoma represents a significant threat to the elderly, with the disease often going unnoticed until it has caused considerable damage. According to the National Eye Survey in Malaysia (NESII), glaucoma is a leading cause of blindness among older adults, necessitating proactive screening measures to mitigate this risk (Chew et al., 2018) [1]. The prevalence of glaucoma and other eye diseases significantly increases with age, underscoring the importance of regular eye examinations for the elderly.
The Impact of Regular Screening
Regular tonometry screenings can dramatically alter outcomes for elderly patients. Early detection allows for timely intervention, which is crucial in managing glaucoma effectively and preserving vision. Studies indicate that regular eye pressure monitoring and subsequent treatment can significantly slow the progression of glaucoma, thereby enhancing life quality and reducing the risk of complete vision loss (Metheetrairut et al., 2002) [3].
Tailored Screening Protocols
Given the heightened risk of glaucoma with age, especially in populations over 60, tailored screening protocols are recommended. These should include annual screenings for those at higher risk, such as individuals with a family history of glaucoma or those who have previously shown elevated IOP levels. This targeted approach ensures that those most vulnerable are monitored more closely, potentially catching glaucoma developments before they result in significant harm.
References
- [1] Chew, F., et al. “Estimates of visual impairment and its causes from the National Eye Survey in Malaysia (NESII).” PLOS ONE, vol. 13, no. 6, 2018, e0198799. [https://dx.doi.org/10.1371/journal.pone.0198799].
- [3] Metheetrairut, Ankana et al. “Evaluation of screening tests and prevalence of glaucoma: integrated health research program for the Thai elderly.” Journal of the Medical Association of Thailand = Chotmaihet thangphaet vol. 85,2 (2002): 147-53. [https://pubmed.ncbi.nlm.nih.gov/12081112].
III. Risk Factors for Glaucoma in the Elderly
Age as the Primary Risk Factor
Age remains the most significant risk factor for glaucoma, with the incidence of this condition notably increasing with each decade after the age of 40. Studies conducted in Indonesia, have shown a direct correlation between aging and the heightened risk of developing glaucoma. This age-related increase in risk is likely due to the natural degradation of eye structures and the accumulation of risk factors over time (Angriani et al., 2022) [4].
The Role of Family History and Genetics
A family history of glaucoma significantly raises the likelihood of developing the condition, underscoring a strong genetic link. In Malaysia, individuals with a known family history of glaucoma are advised to undergo more frequent screenings, as genetic predisposition can lead to earlier and more aggressive forms of the disease. The importance of understanding and acknowledging family medical history cannot be overstated when planning preventive care for glaucoma (Angriani et al., 2022) [4].
Systemic Conditions as Compounding Factors
Systemic health conditions such as diabetes and hypertension are prevalent in Malaysia and contribute significantly to the risk of developing glaucoma. These conditions affect vascular flow and can lead to changes in eye pressure and subsequent optic nerve damage. The interplay between systemic health and eye health is crucial, and managing these conditions is part of preventing glaucoma (Sun et al., 2022) [5].
Addressing Preventable Risk Factors for the Optic Nerve
Lifestyle choices and health-related behaviors also play roles in the risk of glaucoma. Smoking, high blood pressure, and poor diabetes control are modifiable risk factors. Public health efforts in Malaysia aim to educate the elderly about these risks and the benefits of lifestyle adjustments to mitigate their impact on eye health.
References
- [4] Angriani, Novita, et al. “Glaucoma Risk Factors.” Green Medical Journal, vol. 4, no. 1, 2022. [https://dx.doi.org/10.33096/gmj.v4i1.94].
- [5] Sun, Junran, et al. “Prevalence and Risk Factors of Glaucoma Among Chinese People From the China Health and Retirement Longitudinal Study.” Journal of Glaucoma, 2022. [https://dx.doi.org/10.1097/IJG.0000000000002094].
IV. Latest Clinical Studies Supporting Regular Screening for Glaucoma
Impact of Regular Screening on Early Detection
Recent clinical studies emphasize the crucial role of regular tonometry screenings in the early detection of glaucoma. For example, a study analyzing the effectiveness of various screening methods for glaucoma noted that optic disc assessment and non-contact tonometry (NCT) are particularly effective in identifying early signs of the disease. These methods have shown high sensitivity and specificity, making them valuable tools in general practice settings (Sim and Goh, 1999) [6].
Advancements in Screening Techniques
The evolution of screening techniques has significantly enhanced the ability to detect glaucoma early. Modern technologies such as digital imaging and automated visual field testing provide detailed insights into the eye’s condition, improving the accuracy of diagnoses and enabling more effective management of the disease. These advancements support the necessity for regular screenings, especially in populations at higher risk such as the elderly in Malaysia.
Prevalence and Necessity for Targeted Screening
Studies continue to show that the prevalence of glaucoma increases with age. For instance, research in nearby regions like Singapore has demonstrated similar trends, underscoring the importance of targeted screening programs that focus on high-risk groups. These programs have been successful in identifying glaucoma in its early stages, significantly reducing the risk of progression to blindness (Sim and Goh, 1999) [6].
Cost-Effectiveness of Glaucoma Screening
While the debate on the cost-effectiveness of glaucoma screening continues, recent reviews suggest that with the right strategies, screening can be both cost-effective and life-changing, particularly in lower-income areas. By catching the disease early, the costs associated with advanced glaucoma treatment and potential blindness can be significantly reduced, making a strong case for the integration of regular glaucoma screenings into routine healthcare for the elderly (Olawoye et al., 2022) [7].
References
- [6] Sim, D H, and L G Goh. “Screening for glaucoma in the Chinese elderly population in Singapore.” Singapore medical journal vol. 40,10 (1999): 644-7. [https://pubmed.ncbi.nlm.nih.gov/10741193]).
- [7] Olawoye, O., Azuara-Blanco, A., Chan, V. F., Piyasena, P., Crealey, G. E., O’Neill, C., & Congdon, N. (2022). A Review to Populate A Proposed Cost-Effectiveness Analysis of Glaucoma Screening in Sub-Saharan Africa. Ophthalmic Epidemiology, 29(3), 328–338. [https://dx.doi.org/10.1080/09286586.2021.1939887].
V. Advantages of Non-contact Tonometry for Elderly Patients
Non-contact tonometry (NCT) is the preferred method for measuring the pressure inside your eye, particularly in elderly populations. This non-invasive technique, which utilizes a puff of air to flatten the cornea, assesses the pressure of your eye and offers several advantages over traditional contact methods like Goldmann applanation tonometry (GAT). It is specifically designed to measure your eye pressure, making it ideal for accurate and safe screening, especially important in early glaucoma detection. The significance of monitoring the pressure inside your eye using non-contact tonometry cannot be overstated, as it provides a reliable method for assessing the risk of glaucoma without the need for direct contact with the eye.
Non-Invasive Nature
One of the primary benefits of NCT is its non-invasive nature. Unlike GAT, which requires direct contact with the cornea and the use of topical anesthesia, NCT does not involve any physical contact with the eye. This feature is particularly advantageous for elderly patients who may have sensitive eyes or who may be at a higher risk of infections. The non-invasive approach of NCT minimizes discomfort and reduces the risk of transmitting infections, which is crucial in a clinical setting [8].
Speed and Ease of Use
NCT is known for its quick and straightforward procedure. The measurement of IOP can be completed in seconds, which is beneficial for both patients and healthcare providers. This efficiency is particularly important for elderly patients who may have limited tolerance for lengthy medical procedures. The quick nature of the test ensures minimal stress and discomfort for patients [8].
Diagnostic Accuracy
While GAT is often considered the gold standard for measuring IOP, studies have shown that NCT provides comparable accuracy. The precision of NCT has been validated in various clinical settings, making it a reliable alternative to GAT. This is particularly relevant in routine screenings where quick and effective assessment of IOP is required [8][6].
Suitability for Screening Programs
Given its non-invasive and rapid nature, NCT is highly suitable for large-scale screening programs aimed at detecting glaucoma, especially among the elderly. Screening programs can benefit from the ease of use and minimal training required to operate NCT devices, facilitating widespread implementation in community settings or during health fairs [6].
Challenges and Considerations
Despite its advantages, NCT does have limitations. For instance, the accuracy of NCT can be affected by corneal properties such as thickness and rigidity, which may vary among individuals. Therefore, it is important for healthcare providers to consider these factors when interpreting NCT results. Additionally, while NCT is suitable for screening, any abnormal findings should be followed up with comprehensive examinations using standard tonometry methods [8][6].
Conclusion
Non-contact tonometry represents a significant advancement in the non-invasive measurement of intraocular pressure, particularly for the elderly population. Its benefits of being quick, painless, and having a lower risk of infection make it an ideal choice in both clinical and screening settings. However, it is essential to consider its limitations and ensure proper follow-up when necessary.
References
- [8] Ghanbarnia, Mohammad Javad et al. “Age-specific distribution of intraocular pressure in elderly Iranian population and its associated factors.” Caspian journal of internal medicine vol. 14,1 (2023): 112-120. doi:10.22088/cjim.14.1.112. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9878900/
- [6] Sim, D H, and L G Goh. “Screening for glaucoma in the Chinese elderly population in Singapore.” Singapore medical journal vol. 40,10 (1999): 644-7. [https://pubmed.ncbi.nlm.nih.gov/10741193]).
VI. Conclusion: The Critical Role of Tonometry in Preventing Vision Loss Among the Elderly
The Importance of Proactive Screening
Tonometry, especially non-contact methods like air puff tonometry, is an invaluable tool for the early detection and management of glaucoma, one of the leading causes of blindness among the elderly. Regular eye pressure screenings allow for the early detection of changes that may indicate the onset of glaucoma, thereby enabling timely intervention to manage the disease and prevent severe vision loss.
Statistical Support for Regular Screening
In Malaysia, studies have shown that a significant portion of the elderly population remains unscreened for eye conditions that could lead to blindness. For example, findings from the National Health and Morbidity Survey indicate that a large percentage of individuals with diabetes, a risk factor for glaucoma, have never had an eye examination. This lack of screening increases the risk of diabetic retinopathy and glaucoma progressing to advanced stages undetected (Goh et al., 2010) [9].
Call to Action: Schedule Regular Eye Exams
It is crucial for adult children to encourage their elderly loved ones to schedule regular eye exams. Clinics offering non-contact tonometry provide a more comfortable experience for the elderly, making the screening process less daunting and more accessible. By prioritizing regular eye exams, you can help ensure that your elderly relatives maintain the best possible vision and quality of life.
Supporting Regular Eye Health Checks
Ensure that elderly family members understand the importance of regular eye health checks. Discuss the ease and benefits of non-contact tonometry with them, emphasizing its non-invasive nature and effectiveness in early disease detection. By fostering an understanding of these benefits, you can help mitigate any anxiety they may have about eye exams and encourage their participation in regular screenings.
References
- [9] Goh, P., Omar, M. A., Yusoff, A. F. “Diabetic eye screening in Malaysia: findings from the National Health and Morbidity Survey 2006.” Health and Morbidity Survey, 2010. [https://pubmed.ncbi.nlm.nih.gov/20848059].
This Article is Medically Reviewed by Woon Pak Seong

Woon graduated as an optometrist in 1995. After working for 9 years for a chain store and an individual optometry practice, he started Vision Space in 2004 to bring the best in global practices of vision care to customers.
He believes in the principle of continuous improvement and excellence. He enjoys meeting people and encouraging them to enjoy life.
A believer in lifelong learning, Woon loves to give optical training and talks at conferences and fairs. He takes delight in reading journals, magazines and books on how to serve his customers better as well as improving the practice of optometry.
His passion is to help people see clearly, comfortably and maintain good eye health through screening for potential eye diseases.
His specialties include:
1. Solving complex vision problems to help customers see clearly.
2. Helping children slow down their shortsightedness.
3. Fitting special multifocal spectacle lenses.
A fun fact about Mr. Woon: He is a movie buff and enjoys good music and food.
Favourite Quote: “Live life to the fullest.”